Optimizing Healthcare Operations in a Digital World

For healthcare professionals, the concepts of patient care and the health system carry additional weight. From the boardroom, leaders at healthcare organizations make strategic operational decisions that impact the way care is delivered to patients. These decisions are informed by their knowledge of what’s best for the organization as well as an understanding of what it is like to be a patient themselves.
Healthcare is a significant aspect of many individuals’ lives. This may include annual visits to a primary care physician, consultations with specialists, or coordinating complex appointments for a family member. Managing healthcare can be challenging, but it is essential and often unavoidable for most people. So why is it that something so important, is not so easy to navigate? How often have you, as a patient or caregiver, completed a portal registration and showed up for your appointment to then be asked to fill out a paper form with the same information that was captured in your portal? This experience can be frustrating not only for patients, but for the staff too. This one small example has a larger impact on overall patient and employee experience than you might think.
The domino effect in patient experience
The patient’s journey starting with registration (i.e., front-end) through to the billing process (i.e., back-end) is a tightly interweaved chain of processes, each step a domino that needs to be placed in proper alignment for the system(s) to function efficiently. Registration sets the foundation by capturing patient demographic and insurance information that flows into scheduling, clinical documentation, coding, and ultimately billing. When any part of this chain or process step is misaligned, it triggers delays, denials, and rework downstream. For example, if a patient’s insurance information is entered incorrectly at registration, it can lead to denials and costly reprocessing as well as frustrating patients when they get a bill out of turn. Or, if the scheduling systems don’t flag authorization requirements, services may be rendered without approval, leading to non-reimbursable care.
Many healthcare organizations still manage these operations in silos, with fragmented systems and disconnected teams. This is often due to legacy workflows and lack of investment in interoperable technologies, which leads to inefficiency, higher administrative burdens, and poor patient financial experiences. Achieving true efficiency requires treating these processes as a unified system, emphasizing alignment, communication, and shared accountability.
Are you making the most of your electronic systems?
Now that we’ve touched on some key inefficiencies at the onset of a patient’s journey, we want to talk about the functionality of your electronic medical/health record (EMR/EHR) systems. An EMR/EHR may accurately register a new patient, but then incorrectly translate care data from the provider, which results in incorrect billing for the patient, hospital, and insurance provider—leaving everyone involved feeling confused and frustrated.
The objective is to implement unified platforms that connect front-end and back-end operations, establish standardized data entry protocols, and promote cross-functional collaboration through shared KPIs and regular feedback processes. Operational efficiency can be improved by treating these processes as interconnected, emphasizing alignment, communication, and collective accountability.
To start, it is important to carefully assess whether a system adequately addresses the needs of both the patient population and your staff. If any gaps are identified, consider the following key factors to enhance the functions of your electronic systems:
Customize & Configure
- Align and configure administrative (front-end) processes with clinical workflows
- Customize system notifications/alerts, order entry, and documentation tools to reduce clicks for your team and risk of mis-translating data
Integration & Interoperability
- Integrate the system with billing platforms, and telehealth so there is one source of truth for accurate patient information
- Avoid data silos by ensuring data is easily shared between clinical and administrative departments through interoperability
- Automation with real-time data capture and sharing allows for faster access to patient information, leading to a quicker turnaround time for clinical and operational decisions
Engage with Patients
- Leverage automation for communication, scheduling, and reminders, freeing up time for your teams to focus on high-value tasks like proactive care coordination
- Maximize patient access to secure messaging, records, and billing details through enhanced portal options
- Make it easy for patients to build a trusting relationship with their provider and care team(s) in a virtual space with user-friendly portal tools
Stay Connected and Keep Vendors Accountable
- Leverage vendor community user groups to share and communicate between similar organizations to enhance system development and learn about new features and updates
- Work with vendors to resolve issues as they arise and customize the platform to your precise needs to ensure maximum functionality
Continuous Improvement and Feedback Loop
- Establish a governance committee with representation across internal teams and levels to oversee optimization and improvement initiatives
- Identify pain points and best practices by continuously collecting end-user feedback
- Implement feedback to enhance the effectiveness of the tool and communicate the successes and ongoing development
It comes down to being thorough and inclusive. By taking a strategic approach to understanding organizational needs and optimizing your EMR/EHR system to meet them, you can significantly enhance both operational efficiency and patient experience. Thoughtful customization, seamless integration, and a commitment to continuous improvement not only reduces administrative burden but also empowers your staff to deliver higher-quality care. As healthcare continues to evolve, investing in the right digital infrastructure will position your organization to adapt, grow, and lead with confidence.
Turn Healthcare Operations Insights Into Action
But… it’s not just about technology
Optimizing technology isn’t the only thing you can do to improve operations. In addition to focusing on improving the patients’ overall experience, aligning your systems with front-end workflows should drive realized revenue and improve the bottom line. The concept that “better experiences lead to greater satisfaction and improved financial outcomes” is widely known in the healthcare industry. However, organizations may encounter challenges in determining where to start when resources for technology optimization are unavailable.
We suggest starting by looking at your front-end processes. Are these processes streamlined in a way that reduces barriers to care for patients, maximizes the bottom dollar, and supports reimbursement? There are two key buckets that can be assessed when looking at the front end:
Operational efficiencies through process improvement
- Standardize workflows by unifying cross-functional teams and processes to minimize manual tasks and rework, reducing employee frustration and administrative overhead
- Improve staff productivity by allowing staff to spend less time on rework and putting more focus on the patient’s experience by equipping them with tools and training tailored to prioritizing patient needs with empathy, problem solving, and clear communication
- Leverage analytics to identify any bottlenecks through enhanced access to data to catch issues or errors early, reducing rework or digging to find information
Revenue optimization
- Engage with patients early to have thorough financial conversations, increasing their understanding, and adoption of payment policies
- Standardize benefit verification and authorization procedures to provide timely and accurate service information
- Incorporate real-time eligibility and verification protocols prior to services rendered to reduce denials and rework
- Implement processes for precise documentation and coding by providing ongoing staff training and conducting regular audits to identify and correct billing errors, ensuring optimal reimbursement
- Reduce the time-of-service delivery to payment with quicker claim processing by leveraging coding and clinical documentation improvement (CDI) tools and batch billing processes
How does all of this impact your bottom line?
A smooth patient care journey leads to more positive experiences, which increases employee and patient satisfaction scores and drives patient loyalty. Healthcare organizations who prioritize quality patient experience gain the competitive advantage and edge that sets them apart in the industry.
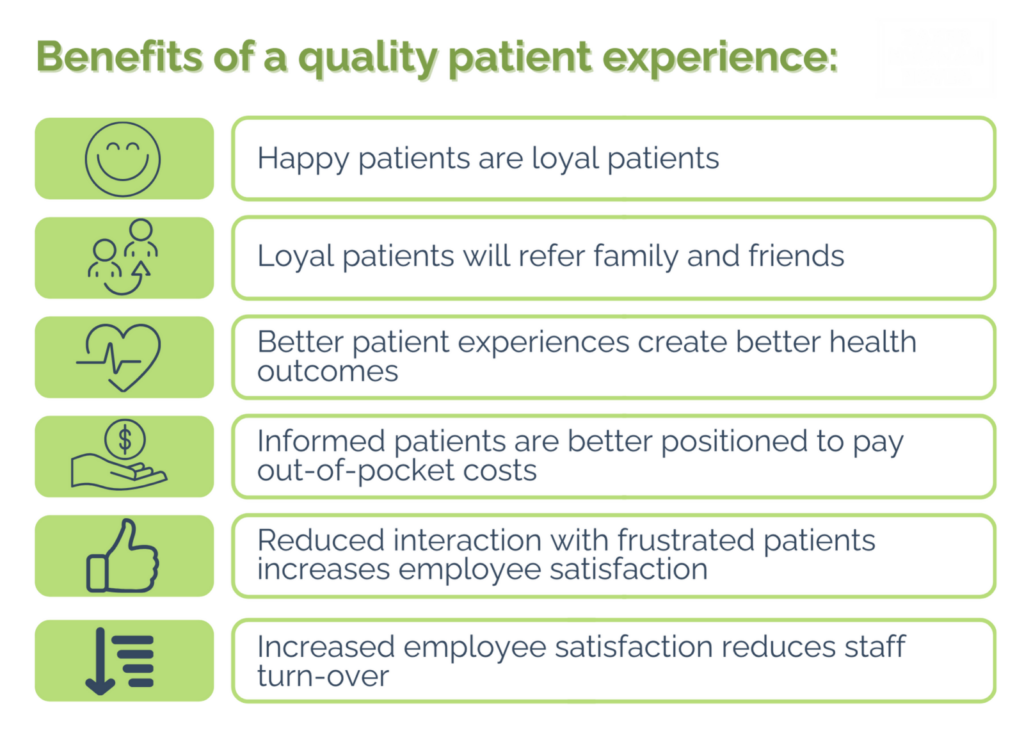
Optimizing your processes and technology to refine the patient care journey ultimately yields efficiencies that financially benefit the organization. Relationships with your patients and care teams will improve with efficient scheduling, timely communication, and transparent billing practices. Automating routine tasks like data entry, appointment reminders, and billing follow-ups reduces labor costs, and the need for overtime or additional hires, potentially saving money in the long-term. By focusing on key areas of opportunity, you’ll protect valuable revenue by maximizing reimbursement, which results in revenue cycle alignment that reduces denials, bad debit, and write-offs.
By building stronger relationships with patients, reducing barriers for patients in accessing their health care information, and supporting them in making informed decisions about their care, your organization not only strengthens its market presence but also stands out as a true differentiator. Now is the time for leaders and stakeholders to come together, evaluate current system performance, and champion the changes needed to drive meaningful improvements. Leadership participation plays a critical role in shaping a more efficient, patient-centered future.
Ready to chat?
In an ever-changing healthcare environment concerned with patient care and access, talent retention and development, and tight financial structures, maintaining efficiency is more important than ever. The BNN BTA team thinks outside the box to reshape your most challenging processes. Whether you’re experiencing clear inefficiencies, have a new need, or are proactively taking a fresh look at your internal processes and workflows, the BNN advisory team can help identify and mitigate risk, support growth and operational effectiveness, and implement solutions that allow your team to focus on what matters most—your patients.
Let's Optimize Your Healthcare Operations Together
Disclaimer of Liability: This publication is intended to provide general information to our clients and friends. It does not constitute accounting, tax, investment, or legal advice; nor is it intended to convey a thorough treatment of the subject matter.